Aging Hearts and Arteries Part III
Click here for Aging Heart and Arteries Part I
Click here for Aging Heart and Arteries Part II
Click here for Aging Heart and Arteries Part IV
Chapter 4: Blood Vessels and Aging: The Rest of the Journey
"A man is as old as his arteries."
Thomas Sydenham, MD, English Physician, 1624-1689
Stretched end-to-end, the arteries, veins, and other vessels of the human circulatory system would measure about 60,000 miles. On any given day, the heart pumps about 1,800 gallons of blood through this vast network. In an average lifetime, the heart pumps approximately one million barrels of blood—enough to fill more than 3 supertankers—through the circulatory system.
No doubt about it, the heart and arteries are remarkable. But as we age, the cardiovascular system becomes more susceptible to diseases including high blood pressure and atherosclerosis. Nearly 40 percent of all deaths among those 65 and older can be attributed to heart problems. By age 80, men are nine times more likely to die of chronic heart failure than they were at age 50. Among women, this risk increases 11-fold over the same time period.
|
Certainly, poor lifestyle—smoking, little or no regular exercise, a diet laden with fat, cholesterol, and sodium—contribute to the development of these cardiovascular disorders. But it is becoming more apparent that like the heart, blood vessels undergo changes with advancing age, and these changes, including arterial stiffening and thickening, are major risk factors for these diseases.
This relationship is complex. In fact, studies—in both animals and humans—have found that many of the factors that underlie the age-related changes in the arteries are also implicated in the development of cardiovascular disease. This suggests that there are some common links between these two distinct, but intertwined processes. Based on these and other findings, some investigators theorize that aging is the driving force in a cycle that begins with age-related changes in the blood vessels. These changes create an environment that promotes arterial stiffening, which contributes to development of hypertension (high blood pressure). | | 
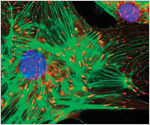
In a healthy artery, the lumen (dark center), where blood flows, is surrounded by arterial wall (red). Age-related changes in the arteries, such as arterial thickening and stiffening,can make them more susceptible to cardiovascular diseases. |
At the same time, age-related changes also make it easier for fatty deposits to build up on the inside of arteries. This accumulation, part of a process known as atherosclerosis, can accelerate the aging of the arteries, which, in turn, leads to further fatty build up and narrowing of the vessel.
In essence, aging arteries form an alliance with risk factors for atherosclerosis, hypertension, and other precursors of heart disease and stroke to profoundly elevate the risk of developing these conditions. However, as scientists learn more about the changes that occur in aging blood vessels, they are making some key discoveries. For instance, in some people these changes occur at an accelerated rate; in others, they occur much more slowly than average. This suggests that how well your arteries perform as you get older depends on a series of complex interactions among age, disease, lifestyle, and genetics, Dr. Lakatta says. In any case, epidemiological studies have consistently shown that people with the greatest amount of arterial stiffening and thickening are at the highest risk for developing stroke, heart attack, and other cardiovascular events.
But investigators also now know that several of these changes, such as arterial stiffening and thickening, don’t occur to the same extent in all people. In fact, studies strongly suggest that exercise, good nutrition, and emerging drug therapies can slow the aging of the blood vessels, even among people who are genetically at risk. These interventions could delay or prevent the onset of cardiovascular diseases in many older people.
“We’re moving into an era when it will be imperative to find out what your blood vessels are like before clinical disease sets in so that, if necessary, appropriate measures can be taken to keep your cardiovascular system as healthy as possible,” Dr. Lakatta says.
In Search of a Connection
So, what made scientists think there might be a connection between stiffening and thickening of arteries and heart function? It goes back to what they have learned in the past few decades, partly through NIA’s Baltimore Longitudinal Study of Aging. By comparing younger and older volunteers, scientists have been able to put together a picture of what happens both in the heart and in the blood vessels as people age.
The heart, they have learned, adjusts in many subtle and interconnecting ways: It develops thicker walls, and it fills with blood and pumps the blood out in a different pattern and even by somewhat different mechanisms than when young. But it is also becoming clear that many of these adjustments are made in response to changes in the structure of the aging blood vessels, particularly the arteries. For instance, NIA studies show that among those with the stiffest arteries, heart walls are thicker.
To picture how these and other changes influence cardiovascular health, imagine an animated computer graphic of the arteries at, say, age 25, when the walls are still fairly smooth, slick, and compliant. As the heart contracts, the aortic valve opens and blood is pumped into the aorta, the largest artery in the body, and flows up toward the neck, where the carotid artery branches off to take blood to the head and brain, and then down toward the rest of the body. When the aorta receives the rushing pulse of blood from the heart, it also receives pressure spreading from the walls of the heart to its own walls. This pressure travels along the aorta’s walls in wave after wave until it reaches the walls of the smaller branching arteries that take the blood to the rest of the body. There, the speed of these pressure waves—known as pulse wave velocity—slows, and some are sent back through the aorta walls, becoming what are called wave reflections.
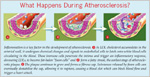
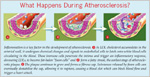
What Happens During Atherosclerosis?|
Atherosclerosis (ath-er-o-skle-RO-sis) is the build-up of fatty deposits called plaque on the inside walls of arteries. Plaque is a combination of cholesterol, other fatty materials, calcium, and blood components that stick to the artery wall lining. A hard shell or scar covers the plaque. As plaque builds up in an artery, the artery gradually narrows and can become clogged. As an artery becomes more and more narrowed, less blood can flow through. The artery may also become less elastic.
Most plaque buildup occurs in medium to large arteries and many investigators suspect that this buildup begins with changes in the endothelium, the innermost layer of the artery. These changes cause white blood cells to stick to the endothelial cells, weakening the barrier between the endothelium and the other layers of the artery. This allows fats, cholesterol, calcium, platelets, and cellular debris to accumulate in artery walls. In turn, this accumulation can stimulate other arterial wall changes that lead to the additional thickening of the endothelium and the formation of plaques.
| | What Happens During Atherosclerosis?
Click here for
larger view |
Plaques have various sizes and shapes. Some plaques are unstable and can rupture or burst. When this happens, it causes blood clotting inside the artery. If a blood clot totally blocks the artery, it stops blood flow completely. This is what happens in most heart attacks and strokes. There are usually no symptoms, such as pain, until one or more artery is so clogged with plaque that blood flow is severely reduced.
All of this takes time. In fact, atherosclerosis is a slow, progressive condition that often starts in childhood. But by age 65 it affects one out of every two adults. Scientists at the National Heart, Lung, and Blood Institute are studying why and how the arteries become damaged with age, how plaques develops and changes over time, and why plaques can break open and lead to blood clots. In particular, they have identified the age-related changes in the arteries discussed in this booklet as the major catalyst for the development of atherosclerosis. Research is underway to find drugs that might delay or prevent these age-related vascular changes and, in turn, reduce the risk of atherosclerosis.
There are a number of other risk factors, such as smoking, high blood pressure, and high blood cholesterol that can be modified with a diet, exercise, and other lifestyle changes. The more risk factors you have, the more likely it is that you have atherosclerosis. Talk with your health care provider about your risks for atherosclerosis and cardiovascular disease and what you can do to reduce them. |
|
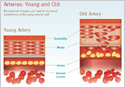
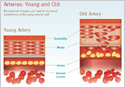
Now, add 50 years to this picture. The arteries, including the aorta, grow stiffer and dilate; their walls become thicker, their diameter larger. As a result, the stiffer vessels no longer expand and contract as much as they once did with each heart beat.Eventually, the opposition to the flow of blood by the stiffer aorta walls increases significantly.
Along the walls of the stiffer aorta, the pressure waves move more rapidly, and as a result, the wave reflections occur sooner than they did before. The timing of the wave reflection, in fact, is one of the effects of arterial stiffness that can be measured noninvasively. Epidemiological studies using these measures have determined that high aortic pulse wave velocity (aPWV) is an independent predictor of arterial stiffness and cardiovascular disease and death.
As the walls of the large arteries become stiffer, diastolic blood pressure tends to drop and systolic blood pressure rises. The difference between these two numbers is called pulse pressure. | | Age and Arteries

Click here for
larger view |
High pulse pressure—greater than 60 millimeters of mercury—is associated with greater thickening and stiffening of arterial walls. In turn, arterial stiffening and thickening contribute to increased pulse pressure. Many studies have found that elevated pulse pressure is also an important risk factor for stroke and heart attack.
Next, picture the effects of movement—when a person sits up, stands up, or begins to walk or run—the heart rate increases and blood pressure changes. A group of pressure sensitive nerves in the base of the carotid artery respond by sending a message to the brain. The brain in turn sends a message back to the heart, which changes its rate and strength of contraction. This arterial/brain/heart message system is called the baroreceptor response.
| Blood vessels also dilate to allow for the extra blood flow. In addition, blood is turned away temporarily from those organs that don’t need it (for instance, the stomach), so that more can be delivered to the working muscles.
In the older picture, the baroreceptor response is blunted with age, perhaps as a result of stiffer arteries. Also, at maximum exercise, the large arteries do not dilate as much as in the younger picture. In essence, this age-related stiffening impedes pulsing blood flow from the heart and places an increased workload on the heart.
As the blood moves into the smaller arteries, the hydraulics change. The pulse smoothes out, the flow becomes more steady. The opposition to this steady flow is known as peripheral vascular resistance or PVR; so far studies show that among men, resting PVR does not change with normal aging, but that it does rise somewhat in women. PVR is actually elevated in people who have high diastolic blood pressure, but is also elevated, to a lesser extent, in people who have high systolic and nearly normal diastolic blood pressure. This condition, called systolic hypertension, is so common that a person age 55 or older has about a 65 percent chance of developing it. However, PVR is not usually directly measured outside of a research laboratory setting because of the complexities involved. Instead, physicians monitor diastolic blood pressure. If it remains steady or increases rather than dropping in the presence of aortic stiffening, it’s a sign of elevated PVR. (See The Nitty Gritty of High Blood Pressure.)
| | 
A sectional view of the arterial wall. On the right is the intima, topped by a layer of cells called the endothelium. The endothelium acts as a barrier to prevent certain substances from entering the vessel wall. In the center, the media is composed of smooth muscle cells and a network of fibrous proteins. The outermost layer, the adventitia, is composed of connective tissue. |
Inside Every Artery...
Scientists are still sorting out why these aging changes in blood pressure and PVR occur and what can be done to prevent them.But one key focal point of research is the inner workings of the arterial wall.
At first glance a large artery resembles a simple rubber tube. But like many first impressions, this is a bit deceiving. The arterial wall is actually comprised of three intricate layers of tissue. The innermost layer, closest to the blood, is called the intima. The part of the intima nearest to the blood is a single layer of specialized cells, called endothelial cells, which sits atop the sub-endothelial space and a wall called the basement membrane. These endothelial cells act as a barrier to prevent certain substances from entering the vessel wall through the intima. Endothelial cells sense mechanical signals, such as blood pressure and flow, and chemical signals, such as oxygen tension, and temperature. In reaction to these signals, they secrete proteins called cytokines and chemokines as well as growth factors and other substances that help regulate the structure and function of the arteries.
The smooth muscle cells in the media, the middle layer of the artery, are surrounded by a network of fibers primarily made of two proteins, collagen and elastin. The elastin forms concentric rings within the vessel wall. The outermost layer, the aventitia, is composed of connective tissue and small blood vessels that feed the walls of large arteries. Together, these three layers of artery wall surround the lumen, the opening that blood flows through on its journey throughout the body. With age, each of these layers change in complex ways.
...Time Takes its Toll
Aging, for instance, triggers thickening of the intima and stiffening of the arterial walls. This occurs, in part, because of a fierce molecular struggle.
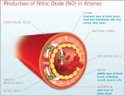
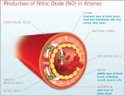
Healthy endothelial cells produce nitric oxide, an important signaling molecule that helps keep arteries supple. When nitric oxide enters a cell, it stimulates a biochemical process that relaxes and dilates blood vessels. Nitric oxide also helps keep atherosclerosis in check by preventing platelets and white blood cells from sticking to the blood vessel walls. The molecule also can curb the abnormal growth of vascular muscle, which can thicken blood vessel walls.
But unhealthy endothelial cells are a different story. In these cells, nitric oxide regulation is impaired. To make nitric oxide, endothelial cells need L-arginine, an amino acid that is one of the basic building blocks of proteins, and an enzyme called nitric oxide synthase (NOS). Normally, endothelial cells have plenty of L-arginine and NOS. But NOS is often in short supply in aging blood vessels. In addition, people who have heart disease or who are at high risk of developing it produce a modified amino acid called asymmetric dimethylarginine (ADMA). ADMA blocks the production of nitric oxide from L-arginine. Even if sufficient amounts of nitric oxide are produced, it can be inactivated by oxygen free radicals, unstable molecules that injure vascular tissue. In any case,without adequate levels of biologically available nitric oxide, endothelial cells in the intima can’t function properly. In fact, some researchers consider decreased availability of nitric oxide in the endothelium as one of the earliest signs of arterial aging and a pathological sign of atherosclerosis and high blood pressure. However, much of this complex process remains a mystery and scientists continue to explore precisely how nitric oxide production and bioavailability affect blood vessels.
The Nitty Gritty of High Blood Pressure|
By age 60, high blood pressure affects one in every two Americans. Hypertension, as doctors call it, was once thought to be a normal part of aging. But researchers now know that high blood pressure is dangerous at any age.
When we talk about blood pressure, what we’re actually referring to is the pressure within the aorta and the large arteries that connect to it. Blood pressure is measured in millimeters of mercury (mmHg) and recorded as two numbers. Systolic blood pressure (the top number in a blood pressure reading) is the maximum pressure that occurs in the blood vessels when the heart contracts. As the heart relaxes between beats, the pressure dissipates. This low pressure is measured as diastolic (the bottom number) blood pressure.
Systolic blood pressure is largely determined by the stiffness of the arteries and the amount of blood pumped through them during a heart beat. Many doctors once believed that as we got older our bodies needed increased systolic blood pressure to push blood through stiffened arteries. But researchers now know that this increase is not normal, and that high blood pressure at any age significantly increases the risk of heart attack, strokes, and kidney failure.
Today, most experts recommend that blood pressure not exceed 120/80 mmHg. Smoking, high cholesterol, and diabetes can elevate the risk of developing high blood pressure. | | 
High blood pressure is more common with age. Getting your blood pressure checked regularly is one of the best ways to detect this condition. Regular aerobic exercise can help keep it within the
normal range. |
Check your blood pressure regularly. If it is elevated, talk with your doctor. Exercise, dietary changes and, in some cases, medication can make a difference.
|
But they do know that endothelial cells depend on nitric oxide to help subdue the production of oxygen free radicals. Nitric oxide molecules can eradicate some of these free radicals, but in the process they also destroy themselves. This leaves less nitric oxide available to help endothelial cells keep arteries in tiptop shape.
|
Angiotensin II, a growth factor involved in this process, is more prevalent in aging arteries. In addition to increasing free radical production, angiotensin II decreases nitric oxide production and stimulates blood vessel inflammation. It also can cause vessels to tighten and raise blood pressure, forcing the heart to work harder.
Much of angiotensin II’s damage is done in partnership with an enzyme called NADPH oxidase, the primary source of free radicals in the arteries. After angiotensin II activates it, NADPH oxidase causes an increase in production of superoxide, a free radical. Superoxide binds with nitric oxide to create an even more potent free radical called peroxynitrite. Peroxynitrite then binds to proteins and nitrites, harming them. Like other free radical processes, this chain of events steals bioavailable nitric oxide away from endothelial cells, leaving them more vulnerable to damage. | | Production of Nitric Oxide (NO) in Arteries
Click here for
larger view | But the impact of angiotensin II isn’t limited to the intima. It also has an important role in age-associated alterations of the media, the middle layer of the arterial wall.
In addition to depleting nitric oxide, free radicals can damage the membranes and DNA of endothelial cells in the intima and smooth muscle cells in the media. Free radical damage is one of many things that can induce some of these cells to stop functioning, shrink, and ultimately die in a process known as apoptosis. Apoptosis may contribute to the decline in cardiovascular health as we age. Free radicals also can oxidize proteins, altering their structure and function. As a result, these proteins can’t work properly, and this can trigger a cascade of cellular alterations that promote stiffening and thickening of arterial walls and contribute to atherosclerotic plaque build up.
|
Stuck in the Middle with You
With age, some smooth muscle cells in the media die causing the remaining ones to work harder and grow larger. Over time, other alterations cause some smooth muscle cells to stop contracting as usual. Instead, these cells begin producing excessive amounts of proteins and other matrix substances, creating an imbalance of elastin and collagen in the media. As the amount of collagen increases in the blood vessel wall, it tends to bind to glucose molecules, forming crosslinks known as advanced glycation end products (AGES). This process, which has been compared to what happens as turkey is roasted in an oven, is slow and complex. But as more AGES form, the collagen strands in the media turn brown, become crosslinked, and become less supple. Age takes its toll on elastin, too. It becomes overloaded with calcium, stretches out, and eventually ruptures, further eroding an artery’s flexibility.
| | Arteries: Young and Old
Click here for
larger view |
Scientists studying this process are particularly intrigued by matrix metalloprotease-2 (MMP2), an enzyme activated by angiotensin II as well as many other signals. Although many of its functions are unclear, studies in rodents, monkeys, and humans suggest MMP2 helps break down key components of the basement membrane, the barrier that separates the intima from the media in artery walls. MMP2, in conjunction with angiotensin II, also activates other growth factors, such as transforming growth factor, which might stimulate collagen and cell growth, the development of fibrous tissue, and contribute to thickening of the intima. In addition, this combination of MMP2 and angiotensin II activates PDGF-B, a growth factor, which acts as an attractant that lures smooth muscle cells to migrate from the media to the intima.
But in smaller blood vessels, the activity of PDGFB and other growth factors, such as vascular endothelial growth factor (VEGF), tend to decline with age. These growth factors play an important role in a process called angiogenesis that leads to the development of new small blood vessels. In some cases, angiogenesis can stimulate the growth of new collateral small vessels around narrow spots or blockages in the arteries that threaten to reduce blood flow to the heart. As we age, however, this process switches off. Enzymes that break down collagen also seem to be involved in this process and are less active as we get older. Scientists are still unraveling why this happens, but as ageassociated changes and damage accumulate in endothelial cells, they secrete less of the critical growth factors needed for angiogenesis. Angiogenesis also depends, in part, on the availability of nitric oxide, which declines with age. In addition, there appears to be an age-associated decrease in the number of endothelial progenitor cells. These adult stem cells are produced in the bone marrow and circulate in the bloodstream.
|
Under certain circumstances, endothelial progenitor cells can differentiate into endothelial cells, which are needed to form new blood vessels or repair damaged ones. In essence, progenitor cells are the “mothers” of “daughter” endothelial cells. As the number of progenitor cells declines, angiogenesis is less likely to occur. Researchers are investigating ways, such as gene and cell therapy, to reactivate angiogenesis in older people who have cardiovascular disease. But scientists have much to learn about the safety and efficacy of these techniques.
From Balloon to Bicycle Tire
Scientists are still piecing together how, or even if, many of these various processes interact. But they do know that, as the result of these and other age associated changes in large arteries, the endothelial barrier in the intima becomes more porous. Some of the signals these cells transmit to the smooth muscle cells in the media become garbled. In turn, these smooth muscle cells can mistakenly perceive that an injury has occurred. They move into the intima, multiply, and produce collagen and other molecules. In reaction, the endothelial cells produce substances that send signals to circulating blood cells to help out in the repair process. Unfortunately, in their effort to help, blood cells stick to endothelial cells instead of flowing smoothly through the blood vessel. The net impact of these interactions is that the intimal-media layer thickens, contributes to arterial stiffness, and creates a fertile environment for the development of atherosclerosis in aging arteries.
| | |
|
Can Gene Therapy be Used to Treat Heart Problems?
In the future an experimental technique, called gene therapy, may allow doctors to treat heart disease and other cardiovascular disorders by inserting a gene into a patient’s cells instead of using drugs or surgery. Investigators are testing several approaches to gene therapy including:
- Replacing a mutated gene that causes disease with a healthy copy of the gene
- Inactivating or “knocking out” a mutated gene that is functioning improperly, or
- Introducing a new gene into the body to help fight a disease.
| | DNA strands

Every day, your body’s cells depend on genes, coded segments of DNA (below), to tell them how to work. Gene therapy is an exciting area of scientific research that one day could help treat inherited and acquired diseases, including cardiovascular disorders.
|
The NIH has been on the cutting edge of this research. More than a decade ago, for instance, cardiovascular investigators began experimenting with ways to increase the supply of certain growth factors through gene therapy. If more growth factors could be produced, scientists theorized they might stimulate angiogenesis—the growth of new small blood vessels called capillaries.
Knowing the genes that code for the growth factors, the investigators found ways to add copies of these genes to heart muscle. To get genes to the myocytes, they engineered molecular delivery trucks called vectors for the genes. These vectors, made from inactivated adenoviruses—the same viral culprits that cause the common cold—were injected into rats. Scientists hoped the vectors would unload their DNA cargo, which then would begin producing the proteins needed to induce capillary growth. And in this experiment, that’s exactly what happened. One of the vectors worked.
More recently, scientists successfully used gene therapy in older rats to increase the activity of the gene that produces calcium pump proteins on sarcoplasmic reticulum, the cellular storage bin for calcium. This therapy significantly improved heart muscle contraction in these rodents. In another animal study, researchers at The Johns Hopkins School of Medicine in Baltimore used gene therapy to convert a small region of guinea pig heart muscle tissue into specialized pace making cells. Potentially, this technique could one day lead to the development of genetically engineered, biological pacemakers to replace implantable electronic devices. However, scientists must overcome many technical challenges before gene therapy will be a practical approach to treating disease.
The NIH has been on the cutting edge of this research. More than a decade ago, for instance, cardiovascular investigators began experimenting with ways to increase the supply of certain growth factors through gene therapy.
|
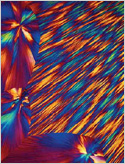
New Blood Test May Help Doctors Detect Emerging Heart Disease
Blood often tells the story of our lives. Tests that measure blood cholesterol levels and other cardiovascular risk factors have become a routine part of health screenings. And in the future, doctors may check yet another blood test—one that measures inflammation—that may help them better assess the risk of disease in the aging heart and arteries.
The test measures levels of C-reactive protein (CRP), a substance produced in the liver, which is often elevated in people who have rheumatoid arthritis and other diseases that cause chronic inflammation. Several studies have indicated that increased blood levels of CRP in otherwise healthy people are associated with an increased risk of heart attack, stroke, and other cardiovascular problems.
Scientists are still investigating whether CRP is merely an indicator of inflammation or if it has an active role in this process. In any case, cardiovascular risk factors such as excessive weight, diabetes, and a sedentary lifestyle are associated with high CRP blood levels. | | Photo of c-reactive protein
Some studies have linked high-levels of C-reactive protein, above, to cardiovascular disease. In the future, a blood test for this substance might help doctors better evaluate a person’s risk of heart attack or stroke. |
| Healthy people with CRP levels less than 1 milligram per liter of blood are considered at the lowest risk of a cardiovascular event in the next 10 years. Depending on medical history and other factors, a person at intermediate risk—1 to 3 milligrams of CRP per liter of blood—could have up to a 20 percent risk of having a heart attack in the next decade. Those with CRP levels of 3 milligrams or more per liter have the highest risk.
However, researchers stress that inflammation is just one of many factors that could increase your risk of cardiovascular disease as you get older. To date no evidence has emerged to suggest that treating people for elevated CRP alone improves survival or reduces cardiovascular complications. For now, detection and treatment of more well-established risk factors, such as high blood pressure and high blood cholesterol, remains a greater priority.
But some treatments for these other risk factors could help lower CRP. The same lifestyle changes, for instance, that help lower cholesterol—regular exercise, a healthy diet, weight loss, and quitting smoking—can also help reduce inflammation. Aspirin and other drugs, including cholesterol-lowering medications such as statins, can decrease CRP levels as well.
...some treatments for these other risk factors could help lower CRP. The same lifestyle changes, for instance, that help lower cholesterol—regular exercise, a healthy diet, weight loss, and quitting smoking—can also help reduce inflammation. |
The cumulative effect of all these age-related changes can be boiled down to this: the ability of larger blood vessels to expand and contract diminishes, the lumen enlarges, and the arterial walls thicken. The result is “hardened”or stiffened arteries that set the stage for the onset of high blood pressure, elevated pulse wave velocity, atherosclerosis, and other precursors of cardiovascular disease. The more severe the effects of aging are on the blood vessels, the easier it is for atherosclerosis, hypertension, and other processes to do damage and, in turn, have an effect on the rate of aging in the vessels. Smoking, lack of exercise, a poor diet, and obesity also can exacerbate these effects.
It’s this cycle, with age as the principal instigator, which gradually helps change youthful and healthy blood vessels into old and potentially diseased ones. In a sense, this progression transforms a young person’s arteries, which are like soft latex balloons, into the equivalent of rigid, bulky bicycle tires in later life.
However, arterial stiffness and intimal-medial thickening occur at varying rates in different people. Studies suggest that the rate of both of these agerelated changes predict stroke, heart disease, and other cardiovascular problems. For example, in one large study that followed healthy volunteers who had no previous symptoms of heart disease, those who had the greatest amount of intimal-media thickening were four times more likely to develop cardiovascular conditions over the next 7 years compared to those with the least arterial thickening. Similarly, studies have shown that healthy people with the stiffest blood vessels were three times more apt to develop high blood pressure over a 5-year span than those with more pliable vessels. In yet another large-scale study, involving 3,075 healthy older people, those who had the highest pulse wave velocity (PWV)—a measure of arterial stiffness—were three times more likely to die of cardiovascular disease than those who had the lowest PWVs.
“Clearly, many people of middle and advanced age whom we once thought of as healthy actually aren’t,” Dr. Lakatta says. “It is becoming more apparent that changes in the aging circulatory system, even among those who don’t have outward symptoms, precede and predict a higher risk of developing cardiovascular diseases. The greater these changes are, the greater is the risk for getting these diseases.”
|
Keeping Your Arteries Healthy
The well-being of your arteries depends on a healthy endothelium, the inner lining of your blood vessels.
“Endothelial cells are the prima donnas within the blood vessels. They control almost every activity that occurs in the vessels, and they’re fundamentally altered with age,” Dr. Lakatta says. “People who maintain a healthy endothelium as they get older and those who make an effort to do things that promote the repair of injured endothelium can reduce the risk of heart attacks and strokes caused by atherosclerosis or hypertension.”
Although scientists still have much to learn about the endothelium and what can be done to keep it healthy, a number of studies suggest that certain modifiable risk factors can have an important impact on the cardiovascular system. | | 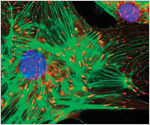
Endothelial cells, such as this one, produce substances that regulate the structure and function of the arterial wall. Endothelial cells may play a critical role in the aging of arteries and the onset of high blood pressure and atherosclerosis. | For instance, regular moderate exercise, such as running, walking, or swimming can reduce body fat, increase lean muscle mass, decrease blood pressure, increase HDL cholesterol (the “good” cholesterol) levels, and lessen the extent of arterial stiffening. All of these exercise-induced changes can have a positive influence on endothelial cells.
In addition, scientists have long known that tobacco smoke contains numerous toxic compounds, such as carbon monoxide, that promote endothelial cell damage. Smoking also increases blood pressure and heart rate. Free radicals in smoke slash the amount of nitric oxide available in the blood stream.Nitric oxide, as you may recall, is a signaling molecule that helps keep arteries pliable. Because nicotine causes narrowing of blood vessels, less oxygen is transported to the heart. If you smoke, blood platelets become stickier and are more apt to form clots in your arteries.
As we mentioned earlier, high blood pressure—hypertension—causes blood vessels to thicken, diminishes production of nitric oxide, promotes blood clotting, and contributes to the development of atherosclerotic plaques in the arteries. Blood pressure is considered high when systolic pressure exceeds 140 mmHg and when diastolic blood pressure is higher than 90mmHg.
Excessive weight increases the risk of high blood pressure and can increase the likelihood that you’ll have high blood triglycerides and low HDL cholesterol, Dr. Lakatta says. Being overweight can also increase the probability you’ll develop insulin resistance, a precursor of diabetes.
Diabetes, a disease in which the body does not produce or properly use insulin, becomes more common as we age. In fact, nearly half of all cases are diagnosed after age 55.Atherosclerosis develops earlier and is more aggressive in people who have diabetes. In part, this occurs because diabetes causes the endothelium to produce excessive amounts of superoxide anion, a free radical that destroys nitric oxide. People age 65 and older who have diabetes are nearly four times more likely than those who don’t to develop peripheral vascular disease, a condition that clogs the arteries that carry blood to the legs or arms.And, cardiovascular diseases and stroke are leading causes of diabetesrelated deaths. If you suspect you have or are at risk for diabetes, check with your doctor. Symptoms include increased thirst, increased hunger, fatigue, increased urination—especially at night, unexplained weight loss, blurred vision, and slow healing of wounds and sores.
|
Exercise: Your Heart’s Best Friend
In one of her better-known gags, comic Ellen DeGeneres quips, “My grandmother started walking five miles a day when she was 60. Now she’s 97 years old and we don’t know where the heck she is.”
Funny, yes. But regular physical exercise is no joke. In fact, it may be the most important thing a person can do to fend off heart disease, stroke, and other age-associated diseases. Emerging scientific evidence suggests that people who exercise regularly not only live longer, they live better.
Scientists have long known that regular exercise causes certain changes in the hearts of younger people: Resting heart rate is lower, heart mass is higher, and stroke volume is higher than in their sedentary counterparts. These differences make the heart a better pump. Evidence now suggests these changes occur even when exercise training begins later in life, at age 60 or 70, for instance. In other words, you don’t lose the ability to become better physically conditioned. In addition, several studies have shown that exercise not only helps reduce debilitating symptoms such as breathlessness and fatigue in people who have heart failure, it also prolongs life.
| |  |
| Exercise training may be effective because it appears to improve the function of virtually every cell in the cardiovascular system. Animal studies, for instance, suggest that regular aerobic workouts help heart muscle cells remove calcium from their inner fluid at a faster rate after a contraction. This improved calcium cycling allows the heart to relax more and fill with more blood between beats.
Exercise also improves blood vessel elasticity and endothelial function, in part, by blocking the production of damaging free radicals and maintaining the production of nitric oxide, an important signaling molecule that helps protect the inner layer of the arteries. Together, these changes can slow the progression of atherosclerosis and other age-related cardiovascular conditions.
Endurance exercises such as brisk walking increase your stamina and improve the health of your heart, lungs, and circulatory system. But other exercises are equally important to maintaining health and self-reliance as you get older. Strength exercises, for instance, build muscles and reduce your risk of osteoporosis. Balance exercises help prevent a major cause of disability in older adults: falls. Flexibility or stretching exercises help keep your body limber. As part of a daily routine, these exercises and other physical activities you enjoy can make a difference in your life as you get older.
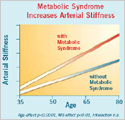
Arterial stiffness, a risk factor for age-related cardiovascular diseases,increases more rapidly in older people who have metabolic syndrome. |
|
Metabolic Syndrome Accelerates Aging of Arteries
Many older Americans have high blood pressure or high blood sugar or just a bit too much fat on the belly. While each of these conditions alone is bad enough, having all of these conditions at once—a cluster called metabolic syndrome—magnifies the risk of developing heart disease and stroke. And NIA scientists may have discovered a reason why: Metabolic syndrome appears to accelerate stiffening and thickening of the arteries.
|
Metabolic Syndrome Increases Arterial Stiffness |
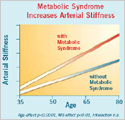 |
Click to EnlargeArterial stiffness, a risk factor for age-related cardiovascular diseases,increases more rapidly in older people who have metabolic syndrome. |
Metabolic syndrome—also known as syndrome X or insulin resistance syndrome—may affect as many as 47 million Americans, according to the Centers for Disease Control and Prevention (CDC). After age 50, a person has a better than one in three chance of developing this group of medical conditions characterized by insulin resistance and the presence of obesity, abdominal fat, high blood sugar and triglycerides, low HDL (good) blood cholesterol, and high blood pressure.
 |
|
Angelo Scuteri MD, PhD | |
|
To determine the effects of metabolic syndrome on aging arteries, NIA researchers studied 471 participants—average age 59—in the Baltimore Longitudinal Study of Aging (BLSA). None of these participants had any detectable signs of cardiovascular disease when initially examined. But those who had three or more conditions associated with metabolic syndrome developed stiffer and thicker arteries at earlier ages than those who didn’t have the syndrome.
“It’s as if the metabolic syndrome makes your blood vessels older,” says Angelo Scuteri, MD, PhD, an investigator at the NIA’s Laboratory of Cardiovascular Science. “If you have metabolic syndrome, when you are 40 your arteries look like they are 55 or 60.”
As this work moves forward, scientists hope they can determine how metabolic syndrome promotes accelerated aging in the arteries and perhaps discover ways to prevent or treat it. |
Researchers have also found that stress reduction techniques, such as taking a walk, practicing yoga, or deep breathing are important to cardiovascular health. Emotional stress triggers the release of adrenaline from the adrenal gland and noradrenaline from the nerve endings in your heart and blood vessels. These hormones make the heart beat faster and adversely affect blood vessels. Under stress, an older person’s blood pressure rises more rapidly and stays higher longer than a younger person’s because the older person’s blood vessels are stiffer and have lost much of their elasticity.
|
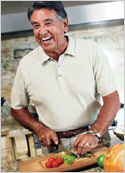
Healthy Foods, Healthy Arteries: Is There a Connection?
What you eat can help keep your heart and arteries healthy—or lead to excessive weight, high blood pressure, and high blood cholesterol—three key factors that increase the risk of developing cardiovascular disease, according to the National Heart, Lung, and Blood Institute. Based on the best available scientific evidence, the American Heart Association (AHA) recommends a diet that includes a variety of fruits, vegetables, and grains, while limiting consumption of saturated fat and sodium.
Fruits and vegetables have lots of antioxidants such as vitamin C and vitamin A that neutralize free radicals and may prevent oxidation in the arteries, dietary experts say. Fruits and vegetables also contain plenty of soluble fiber, a substance that has been shown to reduce blood cholesterol levels, which is healthy for the endothelium.
Breads, cereals, and other grain foods, which provide complex carbohydrates, vitamins, minerals, and fiber, are associated with a decreased risk of cardiovascular disease, according to the AHA Dietary Guidelines.However, some studies suggest eating less sugar, breads, and other simple and complex carbohydrates can lower blood insulin levels and decrease body fat and weight—three factors that are linked to an increased risk of heart disease and stroke. In recent years, a number of dietary recommendations based on these findings have become popular and are currently catching the public’s awareness. While contentious, these are important issues and long-term studies are required to determine the risks and benefits of such diets, Dr. Lakatta says. | | 
Fruits and vegetables are key components of a heart-healthy diet. These food contain compounds that can help subdue free radicals, prevent oxidation in the arteries, and lower blood cholesterol levels, all of which are important for maintaining a thriving endothelium.
|
Saturated fats are usually solid at room temperature. These fats are primarily found in animal foods like meat, poultry, and dairy products like butter. Saturated fats tend to raise levels of “bad” low-density lipoprotein (LDL) and increase the risk of atherosclerosis. In fact, within 2 hours of eating a high saturated fat meal, endothelial cells don’t work as well. Such meals can cause a temporary 50 percent dip in endothelial function, even in healthy young people who have no risk factors for atherosclerosis, Dr. Lakatta says.
In addition to saturated fats, some scientists are concerned about trans-fatty acids—unsaturated fats that have been artificially solidified by food manufacturers in a process called hydrogenation to make products like margarine and vegetable shortenings. These scientists suspect that trans-fatty acids, which are often described as hydrogenated or partially hydrogenated fats on many food labels, are more damaging to the heart and arteries than saturated fats.
|
But researchers have found other types of fats may be beneficial. Monounsaturated fats, found mainly in plant foods such as peanuts and olives, help lower LDL cholesterol. Like polyunsaturated fats, monounsaturated fats are usually liquid at room temperature. Polyunsaturated fats, found in fish, nuts, and dark leafy vegetables, have been getting a lot of attention from scientists in the past few years. They’ve concluded that one type of polyunsaturated fat—omega-3 fatty acid—found in fish may promote several things that improve endothelial function, including increasing nitric oxide production, slashing the production of free radicals and other substances that cause inflammation, and boosting HDL cholesterol levels. Fish such as salmon, herring, and mackerel are good sources of omega-3s.
Control over the condition of our arteries may also lie in how much salt we consume. In cultures where little sodium (in the form of salt) is consumed, blood pressures do not rise with age. Cultural differences have also been found in arterial stiffness. One study compared rural and urban populations in China. The urban population consumed much higher levels of sodium than the rural groups. And they had stiffer arteries. Other researchers found that sodium appears to accelerate age-associated stiffening of arteries. In particular, sodium promotes thickening of aging arterial walls, reduces the amount of nitric oxide available to endothelial cells, and promotes the formation of oxygen free radicals. But shifting to a low sodium diet, research suggests, can begin to diminish arterial stiffness in as little as 2 weeks.
Most of the sodium in your diet comes from processed foods. The remaining is added at the table and while cooking. Scientists who study this issue suggest limiting the amount of sodium that you consume from all these sources to no more than 1,500 milligrams (mg) each day (an average American adult consumes about 3,300 milligrams daily). They recommend reading food labels carefully and buying foods that say “reduced sodium,” “low in sodium,” “sodium free,” or “no salt added.” Some dietitians suggest seasoning foods with herbs and spices like oregano, onion powder, or garlic instead of sodium.
| | 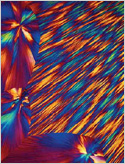
Blood cholesterol, shown here in a crystallized image, is one of many modifiable risk factors that contribute to the onset of atherosclerosis and cardiovascular disease in later life. Dietary changes and regular exercise can help keep blood cholesterol levels under control.
|
Scientists suspect the more lifestyle changes, including diet and exercise, you can incorporate into your life, the better off your arteries will be, because these interventions work independently as well as in unison to promote the vitality of endothelial cells and contribute to reducing the risk of cardiovascular disease.